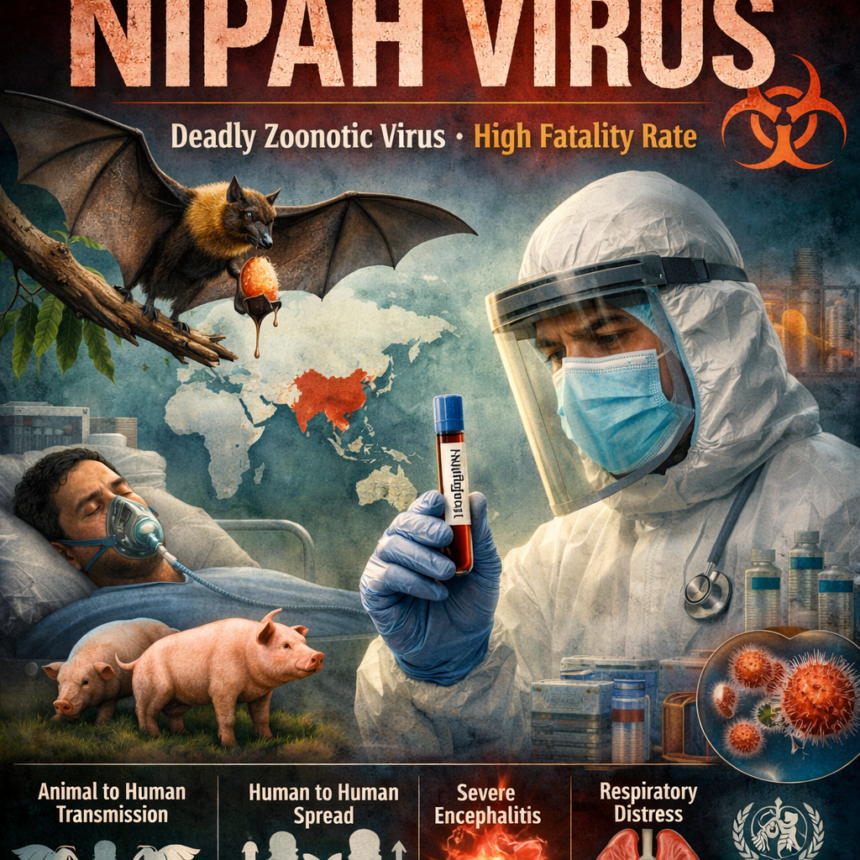
The Nipah virus (NiV) is a highly dangerous zoonotic virus that has emerged as a serious public health threat in parts of Asia, particularly South and Southeast Asia. Known for its high fatality rate and lack of specific treatment or vaccines, the Nipah virus continues to worry health authorities worldwide. Since its first identification in the late 1990s, sporadic outbreaks have caused severe illness and death, highlighting the urgent need for awareness, surveillance, and preparedness.
Origin and Discovery of Nipah Virus
The Nipah virus was first identified in 1998–1999 during an outbreak among pig farmers in Malaysia and Singapore. The virus was named after the village of Kampung Sungai Nipah in Malaysia, where one of the earliest cases was detected. Scientists later discovered that fruit bats of the Pteropus genus, commonly known as flying foxes, are the natural reservoirs of the virus. These bats can carry the virus without showing symptoms and can transmit it to other animals and humans.
How Nipah Virus Spreads
Nipah virus is primarily transmitted from animals to humans, but human-to-human transmission has also been documented. The main modes of transmission include:
-
Direct contact with infected animals, especially pigs
-
Consumption of contaminated food, such as raw date palm sap contaminated by bat saliva or urine
-
Close contact with infected individuals, including exposure to body fluids like saliva, urine, or respiratory droplets
Healthcare settings are particularly vulnerable during outbreaks, as caregivers and medical staff can become infected if proper infection control measures are not followed.
Symptoms and Clinical Impact
The incubation period of Nipah virus typically ranges from 4 to 14 days, though in some cases it can be longer. The infection often begins with non-specific symptoms such as:
-
Fever
-
Headache
-
Muscle pain
-
Vomiting and sore throat
As the disease progresses, it can lead to severe neurological and respiratory complications. Patients may develop acute encephalitis (inflammation of the brain), drowsiness, disorientation, seizures, and in extreme cases, coma. Respiratory distress may also occur, increasing the risk of transmission.
One of the most alarming aspects of Nipah virus infection is its high case fatality rate, which ranges between 40% and 75%, depending on the outbreak and healthcare response. Some survivors also experience long-term neurological complications.
Nipah Virus in India
India has reported several Nipah virus outbreaks, particularly in the state of Kerala. The first outbreak occurred in 2001 in West Bengal, followed by multiple outbreaks in Kerala since 2018. These outbreaks prompted swift public health responses, including isolation of patients, contact tracing, and community awareness campaigns. Kerala’s experience has been widely praised for its effective containment strategies, despite the limited medical options available.
Diagnosis and Treatment
Diagnosing Nipah virus infection requires specialized laboratory tests, such as RT-PCR, ELISA, and virus isolation, which are conducted in high-containment laboratories due to the virus’s extreme risk level.
Currently, there is no specific antiviral treatment or approved vaccine for Nipah virus. Medical care is largely supportive and focuses on managing symptoms, maintaining vital functions, and preventing complications. Experimental treatments, including monoclonal antibodies and antiviral drugs, are under research, but none are yet widely available for routine use.
Prevention and Control Measures
Preventing Nipah virus outbreaks relies heavily on public awareness and preventive strategies, such as:
-
Avoiding consumption of raw date palm sap
-
Preventing bats from accessing food collection areas
-
Using protective equipment when caring for infected individuals
-
Implementing strict infection control practices in healthcare settings
-
Monitoring animal health and reducing contact with infected livestock
Community education plays a crucial role in reducing risky behaviors and early reporting of symptoms.
Global Health Significance
The World Health Organization (WHO) has listed the Nipah virus as a priority pathogen due to its epidemic potential and lack of effective countermeasures. With increasing human-animal interaction, deforestation, and climate change, the risk of zoonotic diseases like Nipah virus is expected to rise. This makes global collaboration, research funding, and surveillance systems more important than ever.
Conclusion
The Nipah virus remains one of the most dangerous emerging infectious diseases in the world. Its high mortality rate, potential for human-to-human transmission, and absence of a proven cure make it a serious global health concern. While outbreaks are currently localized, the threat of wider spread cannot be ignored. Strengthening public health systems, promoting awareness, and investing in research are essential steps to protect communities and prevent future outbreaks of this deadly virus.